What are the treatment and prevention implications of the Nose 1st/Lung 2nd Model of COVID-19 pneumonia?
June 29, 2020
Contributed by Dr. Ashley Haase, MD, Regents’ Professor and Head, Department of Microbiology and Immunology; Professor of Medicine Infectious Diseases and Internal Medicine
In “SARS-CoV-2 Reverse Genetics Reveals a Variable Infection Gradient in the Respiratory Tract,” Hou et al. (Richard C. Bucher and Ralph S. Baric at the University of North Carolina are the corresponding authors) map the expression of the SARS-CoV-2 ACE-2 receptor from the upper to the lower airways. They show that there is a gradient of expression in the normal human upper and lower respiratory tract, with the highest levels in the nose and, in descending order, bronchi, bronchioles and finally alveoli. SARS-CoV-2 infection in cultured cells paralleled receptor expression, with highest infectivity in nasal epithelial cell cultures and lowest in alveolar type 1 and 2-like pneumocytes (Figure 1).
Moving to in vivo studies of COVID-19 pneumonia in lungs from individuals who succumbed to infection, the authors report that the lung infection has the characteristics of an aspiration pneumonia in which SARS-CoV-2 had infected Type 1 and 2 pneumocytes, just as had been the case in vitro, in cultured cells. Putting it all together, the authors propose in the Nose 1st/Lung 2nd model (Figure 1) that infection begins in the nose and upper airways. Aspiration of infectious inoculum then seeds and establishes the second phase lung infection.
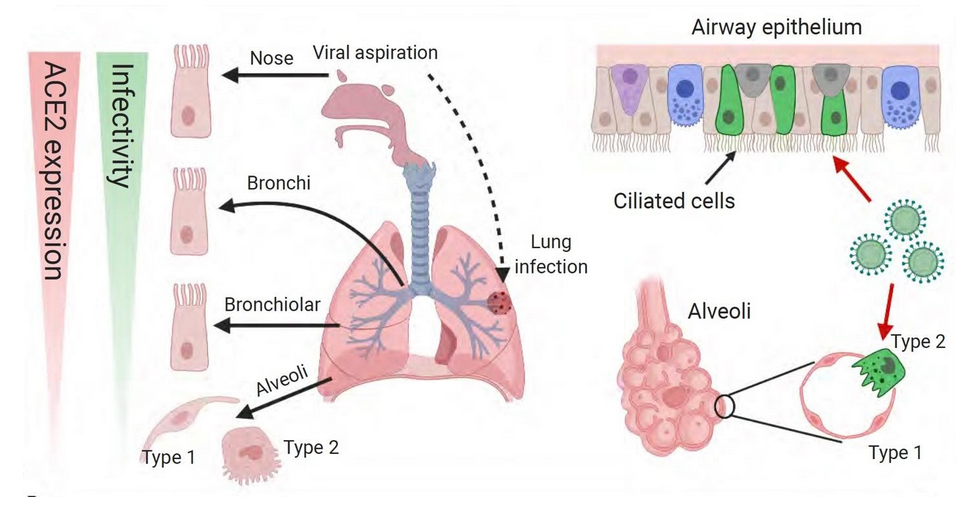
Fig 1 Nose 1st/Lung 2nd Model of COVID-19 pneumonia. The gradient of SARS-CoV-2 ACE-2 receptor expression governs the types and order in which cells are infected. Because receptor expression and infectivity are highest in the nose and upper airways, the model proposes that infection starts there. The second stage of lung infection is initiated by aspiration of the virus produced in the nose and upper airways. The arrow points to a focal patchy lung infection at the periphery characteristic of aspiration pneumonia. The right side of the Figure shows SARS-CoV-2 virus infecting the ciliated cells that line the airways and Type 1 and 2 pneumocytes that line the alveoli.
Coming back to the question of the implications of the model for treatment and prevention, the authors speculate that their findings favor nasal infection as the dominant mode of transmission by aerosol particles in the size range exhaled during normal breathing. Virus production in nasal secretions are mixed with oropharyngeal/tonsillar fluid aspirated into the deep lungs, which initiates lung infection in some individuals. This model “argue[s] for the widespread use of masks to prevent aerosol, large droplet…exposure to the nasal passages” and that “therapeutic strategies that reduce viral titer in the nose early in the disease… may be beneficial.” I would add my personal speculation, that because of the initial focal nature of the lung infection, early antiviral treatment could prevent progression to severe COVID-19 pneumonia as well.