The need for clinical education to train future health care professionals doesn’t stop during a pandemic.
When Minnesota Governor Tim Walz called on Minnesotans to remain at home for a two-week shelter-in-place period beginning on March 27, faculty in the University of Minnesota Medical School and School of Nursing swiftly adapted. With clinical experiences halted by the pandemic, faculty members turned to telehealth as a new model for clinical education.
For health care systems across the United States, the shelter-in-place order meant halting routine or elective care while health systems prepared for the demand for emergency and intensive care needs for COVID-19 patients, as well as preserving personal protective equipment.
NECESSITY ENCOURAGES CREATIVE PROBLEM-SOLVING
Although telehealth had existed prior to COVID-19, it was an underused technology and resource. With the pandemic as a disruptor, along with the legislative and regulatory policy changes it brought, years of anticipated growth were implemented within weeks as telehealth expanded and was adopted.
For clinical education, the change was even more accelerated. “Before the pandemic, there was minimal telehealth education for medical students and residents,” said Joshua Thompson, MD, MPH, a family medicine physician with University of Minnesota Physicians and assistant professor in the Department of Family Medicine and Community Health. “There were a few existing telehealth programs such as tele-stroke and tele-ICU, but most of our physicians were not participating in telehealth, so this was a big pivot for us at the start of the pandemic.”
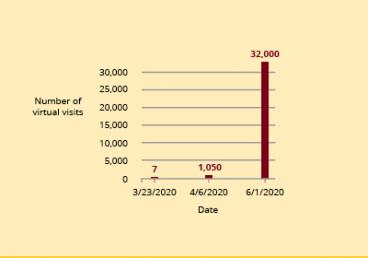
The statistics speak volumes. The University of Minnesota health system partner M Health Fairview went from delivering seven virtual health care visits on March 23, 2020 to more than 1,050 on April 6, 2020. By June, 80 percent of its health care visits were virtual. The rapid expansion of telehealth offered advanced practice nursing students, medical students and medical residents with vital clinical rotations during a time when on-campus learning was paused. More than 100 advanced practice nursing students, medical students and medical residents resumed clinical rotations and delivered patient care during the early days of the pandemic.
The foundation was in place for the School of Nursing and the Medical School to make this rapid transition.
“Before COVID-19, we had an objective structured clinical examinations (OSCE) structure in the curriculum and we’ve had an awareness of telehealth for some time,” said Mary Benbenek, PhD, APRN, FNP-BC, CPNP-PC, FAANP, a clinical professor in the School of Nursing. “History is approximately 85 percent of your diagnosis and telehealth really emphasizes that and helped us prepare to convert OSCEs to telehealth visits.”
Although the rapid transition to telehealth brought challenges, including logistical and technological hurdles, the response from medical students and residents was positive.
“With a telehealth visit, we are forced to hone in on verbal communication skills,” said Thompson. “With the increasing number of diagnostic tests available to us as clinicians, it’s easy to see that as perhaps less important in some situations. Telehealth visits encourage learners to develop and fine-tune that skill set.”
For the School of Nursing, telehealth gave second- and third-year nursing students the opportunity to meet required clinical hours.
“When the opportunity came up, we were so grateful,” said Benbenek. “I felt that the students and patients adapted very readily. These experiences may have improved their ability to ask questions—and this type of care helps develop the ability to see the early presentation of an illness. Many of our nurses have done telephone nurse triage in the past, so that background was very helpful.”
In the process of expanding telehealth, Thompson noted that the number and diversity of patients willing to participate in telehealth visits brings great promise to the future of virtual care.
“Patients who we thought may not want to participate in telehealth, including older patients, were incredibly willing and able to embrace these changes right along with us,” said Thompson.
According to Thompson, telehealth visits peaked early in April and May and the pendulum to in-person care slowly began swinging back once the health systems were able to resume in-person care.
“We expect that telehealth visits could once again increase again during the fall and winter when we see more of the respiratory viruses that we regularly see during these seasons,” said Thompson.
“It’s almost a revolution in care delivery,” said Benbenek. “We all had to change quickly and that’s what was so impressive. Patients adapted very quickly, and they deserve great credit for this. If we work together, we can address our challenges and achieve great things.”
INTERPROFESSIONAL COLLABORATION CRITICAL TO SUCCESS
One key factor for the success is the University’s commitment to interprofessional collaboration.
“This will be a part of our nursing practice going forward,” said Benbenek.
Associate Vice President for Clinical Affairs Carolyn Porta, PhD, MPH, RN, FAAN, convened a Telehealth Education and Clinical Training Workgroup to centralize valuable tools and resources on telehealth education and clinical training.
Faculty members are using best practices to incorporate telehealth clinical education into the curricula, including work with the University’s M Simulation team to offer simulation-based educational opportunities.
Thompson gives great credit to the partnership between the University of Minnesota, University of Minnesota Physicians and its health care system partner M Health Fairview.
“Our health system has done an incredible job supporting this transition,” said Thompson. “We moved from being able to do a handful of visits within a week to doing thousands. We moved mountains and it was inspiriting to see how the technology invested made clinical education excel during this challenging time.”